Hello all,
It’s me, Nor! If you haven’t already met or heard about me, I am the newly-appointed Programmes Manager at Project X. I’ve been with the team for a little more than 6 months and I can’t say enough how much it’s been my greatest pleasure to work in an organisation like Project X. The learning curve has been steep, but I find myself deeply humbled and in service to the communities that Project X caters to. Now that’s out of the way, I’m excited to share about my recent adventures in London!

On the 22nd and 23rd September, I had the opportunity to attend the Life Beyond HIV Conference in London (LBHiV for short), courtesy of Gilead. This year, the conference was a hybrid meeting in every sense of that word. While meetings happened online and physically, it was also a hybrid meeting of disciplines and practices concerning public health. There were physicians, holistic practitioners and advocates from all over the globe.
This year, the conference focused on person-centred care and improving the quality of life (QoL) of people living with HIV. As this was the first ever public health conference I attended, I was eager to learn and hear of the strategies taken by other health practitioners and non-profit/non-governmental organisations in providing access to sexual health care and services.
What does person-centred care mean within the HIV/AIDS context? The welcome address Enabling Every Person Living With HIV To Live Their Best Life by David Wohl, Catarina Esteves and Susan Cole clued me in on the challenges PLHIV faced in accessing diagnosis, HIV care and treatment. Barriers to testing, taking treatment and staying engaged in healthcare settings included anticipated stigma, self-stigma, discrimination and disadvantage.
“People who are closest to the pain should be closest to the power”
During the conference, I was placed under the advocacy track. It was very inspiring and empowering that in most of the masterclasses I attended, they were led by women living with HIV. Most of these women previously faced difficulties accessing adequate HIV care and made it their lives’ work to remove the barriers that can enable a higher quality of life.
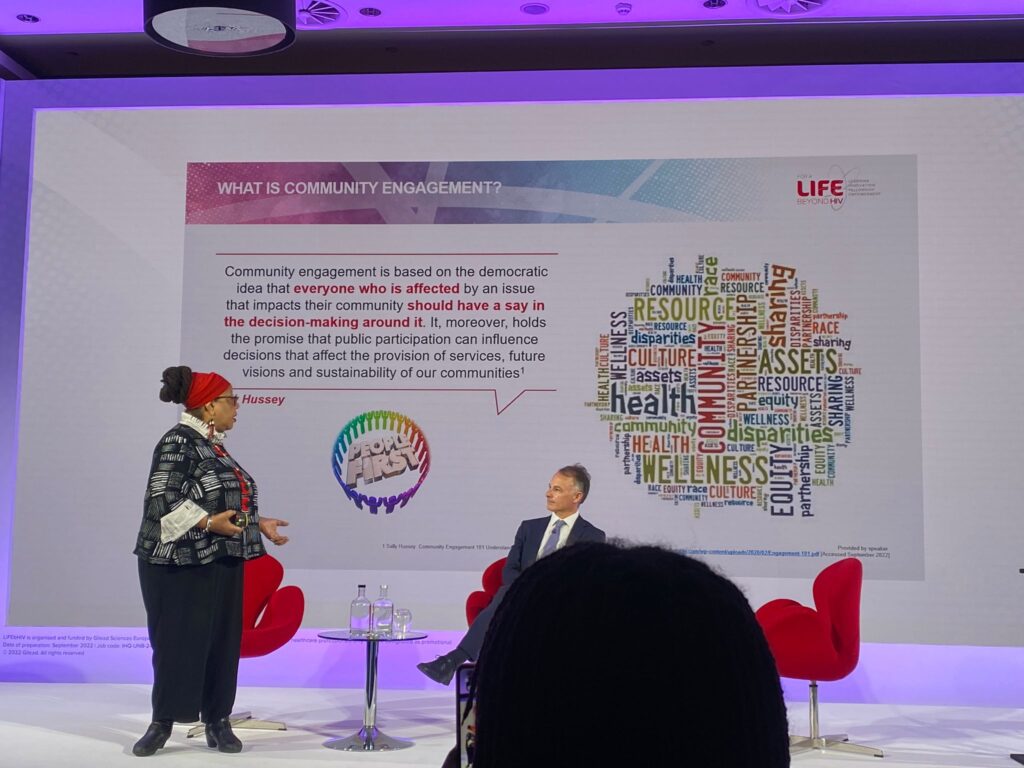
Person-centred care can also mean for healthcare providers to respond to specific needs of people living with HIV through patient-reported outcomes (PROMs). People with HIV are not passive and voiceless. PROMs can be used to enable healthcare providers to prioritise based on a person’s current needs and help identify stigma and discrimination in specific care settings or at a national level. In her presentation, Dazon Diallo, founder of Sister Love, Inc. shared about community engagement approaches and a human rights framework towards policy advocacy. She quoted Sally Hussey in her presentation, stating that “everyone who is affected by an issue that impacts their community should have a say in the decision-making around it”. This means helping them to access the care they need, when they need it, by involving them in their own care decisions.

Some challenges she pointed out included health disparities, unemployment, homophobia, sexism, stigma, criminalisation of HIV, drugs and homelessness. Bruce Richman drove this point further in his presentation by emphasising that “Housing is healthcare”. Homeless folks as well as people living in compromised housing situations may not be able to comply with necessary HIV care. They may not be able to have their medicine delivered, safekept or place their medicine in a visible position that reminds them to take their medication.
The New Normal?
The Covid-19 pandemic resulted in major changes being made to HIV Care and treatment. Sanjay Bhagani and Maka Gogia shared about strategies taken in different countries. At the height of the pandemic, HIV was perceived as a lower priority in health systems. This resulted in patients’ inability to make health consultations, difficulties containing tests, reduced access to PrEP as well as increased stress, anxiety and even substance use.

These challenges resulted in technology-based innovations for consultations, home delivery of ART (anti-retroviral therapy) and multi-month dispensation as well as strengthened partnerships between healthcare organisations and grassroots community groups. However, the lack of face-to-face time and increased use of technology also meant that there was a challenge in addressing wellness beyond physical health such as psychosocial services.. Vulnerable and socially disadvantaged groups became hard to reach during the pandemic due to the lack of access to technology-enabling methods of care. Maka Gogia shared that in Georgia there was a concerted effort to work with community organisations to support internet access or access to smartphones and tablets for online consultations.
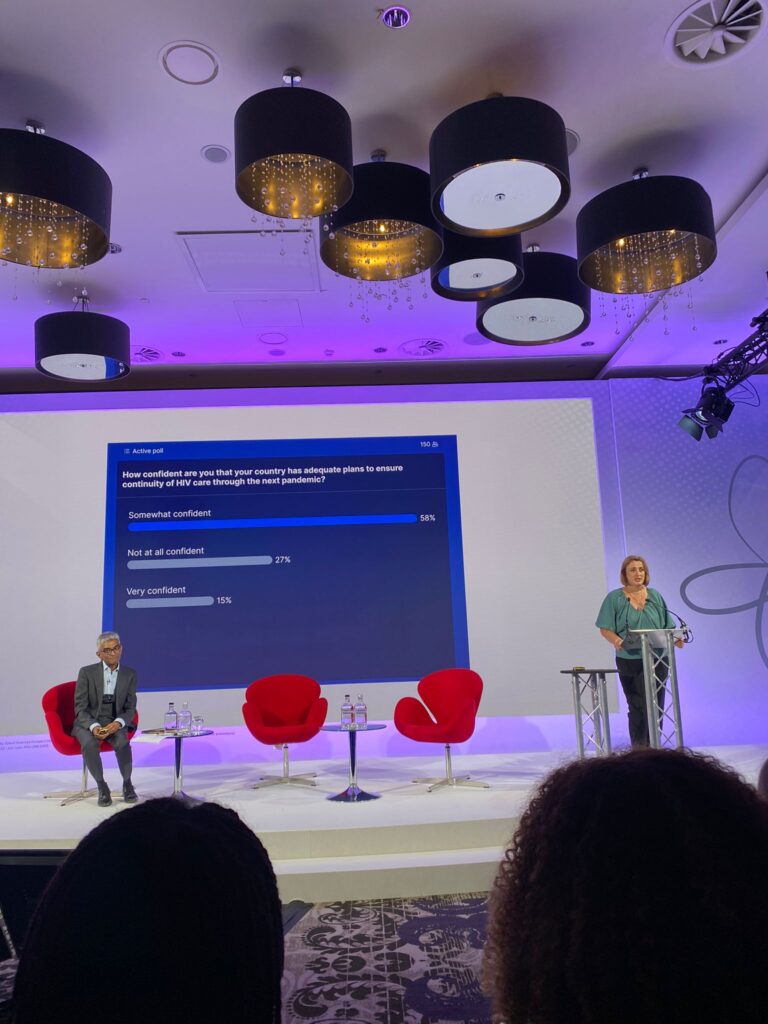
Having access to digital devices and internet access is a privilege that should never be taken lightly, especially in a “post”-pandemic world. By the end of Bhagani and Gogia’s sharing session, the audience was asked if our home countries were well prepared for the next pandemic.
Comprehensive HIV care cannot happen if societal and legal impediments to effective HIV response are not removed. The first day wrapped up by reinforcing that person-centred care puts the individual at the centre of their care.
Stigma
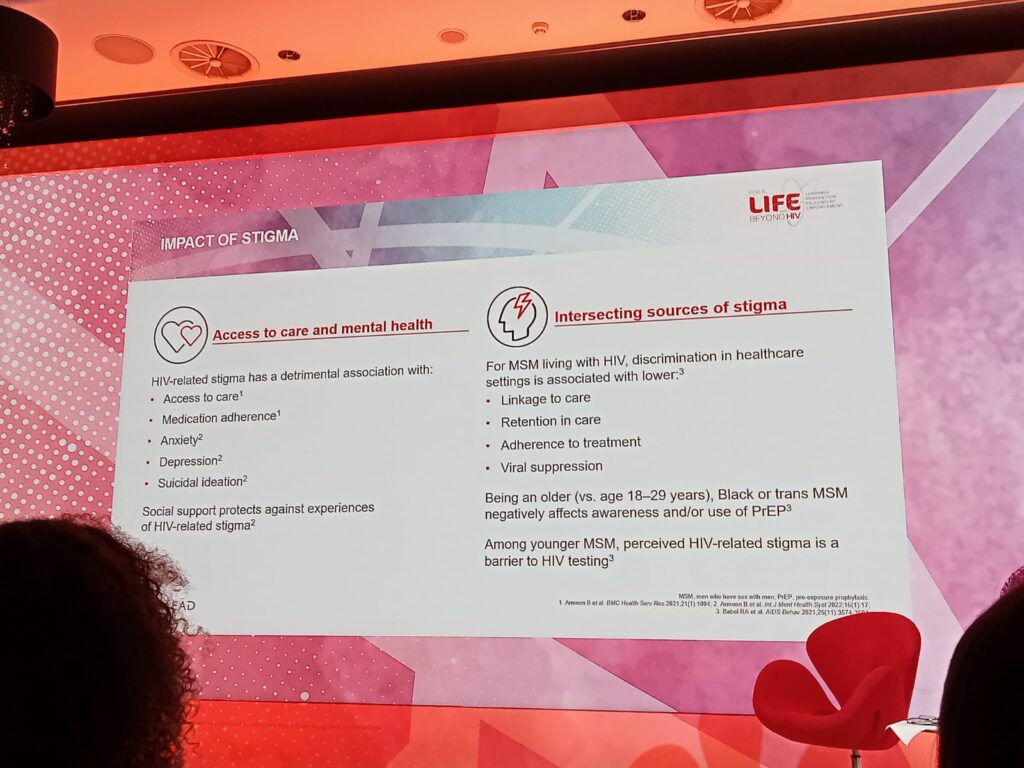
Throughout different sharings, stigma was identified as one of the biggest barriers to HIV diagnosis and care. Self-stigma – a type of stigma – is internalised and perpetuated through structural policies such as the criminalisation of HIV in 92 countries (as of 2020), healthcare staff feeling at risk of transmission when treating a patient with HIV, to downright rejection by the community in situations such as not wanting to date or have sex with people living with HIV. HIV-related stigma is detrimental to access to care, medication adherence, and leads to anxiety, depression and suicidal ideation.
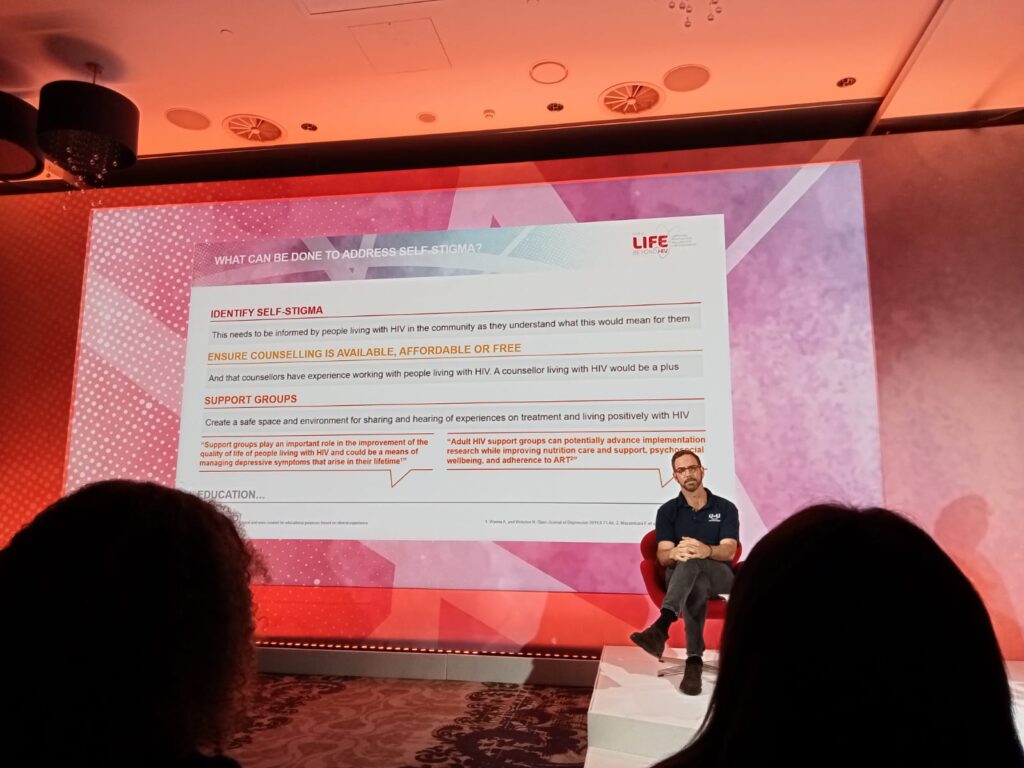
Addressing self-stigma can be made possible through its identification and understanding what it means to each person living with HIV, supported with affordable and/or free counselling as well as support groups.
One such example is the U=U movement, a collaborative and community-led initiative between medical organisations and advocacy groups. Adopting the U=U movement is a beam of hope in dismantling stigma. With the advent of modern antiretroviral therapy, people living with HIV can manage their viral load to the point of it being undetectable. When the viral load is undetectable, this means that HIV is untransmittable. This means good news especially for partners of people living with HIV and parents with HIV who intend to have children.
Despite the science supporting U=U, there are gaps in mainstream awareness due to stigma and scepticism even among healthcare practitioners. It is heartening to hear towards the end of the conference that in Southeast Asian countries such as Thailand and Vietnam, concerted efforts are being made to make U=U accessible to the general public, through mainstream media and popular culture such as variety shows and commercials. In Vietnam, the U=U message has even been adopted and tailored to its specific cultural context, known as K=K. Vietnam is the first country in the world to develop and implement U=U on a national level! The U=U movement is testament of change that can happen, especially when movement is led by the people affected most and supported by advocacy circles, healthcare providers and boosted through systemic support from the government.
To me, person-centred care means to care for a person living with HIV holistically – to think of their needs beyond just prioritising their physical health, but also ensuring they are living their best life, resulting in reduction of further transmission. Beyond just access to affordable antiretroviral therapy, access to housing, being around non-judgmental and affirming support systems, access to technological devices and data that allows them to stay connected with healthcare providers and mental health wellness should all also be considered. While it was a short 2-days conference, I learnt so much that further affirmed the approaches that are already put into practise at Project X. I am hopeful of the direction and potential of our community advocacy groups and the initiatives taken by healthcare providers to be sensitive towards the needs and concerns of people living with HIV in Singapore.
—
Nor is the Programmes Manager at Project X since April 2022. They handle administration for our key programmes and services, facilitate support group sessions and ensure that our drop-in centre is conducive for healing and connecting with others.
Nor firmly believes in self-determination and interdependence, both of which are values that align with the work that Project X does.